…by Nick Jaworski…
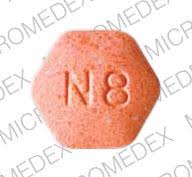
After nearly 80 years, addiction treatment in America is slowly warming to the idea of multiple pathways to recovery, after viewing the 12 steps as the only “real” way to recover. MAT (medication-assisted treatment) is among the most promising.
This is a guest-post by Nick Jaworski, owner of Circle Social Inc., a marketing and consulting firm specializing in addiction treatment. (See bio information at bottom)
……………………
Quite recently, MAT has gained recognition as the gold standard for care in treating opioid use disorder (OUD) among researchers, legislators, and even the general populace. But the acceptance of MAT by the professional treatment community has not been nearly as fast.
Many providers I speak with are still very reluctant to accept MAT in their centers or as a viable component of treatment within the field in general. Even if facility leadership is on board, there’s a good chance staff or referral partners won’t be.
Other providers, such as Hazelden, were also reluctant at first but looked at the research and made their own determination that they had to change their approach (other providers, even today, still look down upon them for it).
Congress and many States have also recognized the efficacy of MAT and so have begun to pump serious money into programs that offer it (like this large grant from SAMHSA). Insurance providers often prefer MAT as well.
Cost is a very significant factor for legislators and insurance providers. MAT protocols can be provided to those struggling with opioid addictions at a fraction of the cost of a residential program ($4,000 or less a year versus $28,000 a month for your average residential program).
Since the majority of those struggling with addiction lack resources or are on Medicaid, MAT also opens the doors for the demographic with the greatest need to access care.
There are two additional drivers of the increase in the use of MAT in the US — Wall Street and parents.
Wall Street has seen great opportunities because the opioid crisis is constantly in the news and the addiction treatment industry has an estimated market cap of at least $35 billion per year. These investors come from outside the field and do not have the same biases. They look at the data and see what’s effective and where trends are going.
And then there are the parents referring their adult children into treatment. Many parents, especially mothers, have become completely disenchanted with the addiction treatment industry as it has existed since the late 1990’s.
Their Children Are Dying from Overdoses, and Parents Aren’t Taking It Lying Down
 The bottom-line is that length of care is one of the highest predictors of success for treatment, so any 28- to 90-day program has very slim chances of success for the first round or two of treatment, regardless of what model they are using. To move away from abusive substance use requires extensive development of new neural pathways that drive new habits and patterns of thought.
The bottom-line is that length of care is one of the highest predictors of success for treatment, so any 28- to 90-day program has very slim chances of success for the first round or two of treatment, regardless of what model they are using. To move away from abusive substance use requires extensive development of new neural pathways that drive new habits and patterns of thought.
As outlined in my article on a Brief History of Addiction Treatment Marketing, it was not uncommon for these young adults to go through 10-plus rounds of treatment. My team and I actually just interviewed a client who was currently on his 27th round of treatment!
As you can imagine some parents have become extremely skeptical after 10-plus rounds of failed treatment (not to mention that they’re paying as much as $30,000 a pop). But, more importantly, many parents have lost children to  opioid overdose. The 18-26-year-old age demographic has always had the highest prevalence of drug and alcohol abuse. Most of the time, this is alcohol or marijuana, with smaller percentages using meth, cocaine, and other substances.
opioid overdose. The 18-26-year-old age demographic has always had the highest prevalence of drug and alcohol abuse. Most of the time, this is alcohol or marijuana, with smaller percentages using meth, cocaine, and other substances.
 However, with the rise in availability of opioid-derived prescription pills, more young adults were switching to these painkillers, which have a high potential for overdose when mixed with other drugs. A subset of these users would go on to heroin, especially when prescription regulations reduced the availability of legal drugs. As most readers know, the extremely high overdose rates of the last few years have been driven primarily by fentanyl-laced (or -replaced) heroin. Unlike
However, with the rise in availability of opioid-derived prescription pills, more young adults were switching to these painkillers, which have a high potential for overdose when mixed with other drugs. A subset of these users would go on to heroin, especially when prescription regulations reduced the availability of legal drugs. As most readers know, the extremely high overdose rates of the last few years have been driven primarily by fentanyl-laced (or -replaced) heroin. Unlike  in the past, when young adults using drugs or alcohol mostly survived to go on and live normal lives (probably like most of those reading this blog), these kids were dying instead.
in the past, when young adults using drugs or alcohol mostly survived to go on and live normal lives (probably like most of those reading this blog), these kids were dying instead.
So parents were sending their children to multiple rounds of rehab, paying tens of thousands of dollars, and then losing their children to overdose anyway. As you can imagine, this created a lot of anger and resentment.
But that was nothing compared to the anger many parents felt when they learned there was this option called MAT that decreased overdose deaths by roughly 40-60% and they had never heard about it! It’s not uncommon for parents who have lost a child to overdose to tell me that the first time they’d heard about MAT was after their child’s death.
Imagine how you would feel if you sent your child to the hospital and you weren’t even told of a readily available and cost-effective method of preventing your child’s death because the doctor personally didn’t care for the treatment.
This is the kind of anger we see from parents such as Gary Mendell, who created Shatterproof, or Justin Phillips, who created Overdose Lifeline. Parents are simply giving up on the traditional rehab industry as a whole because they feel lied to.
American Addiction Treatment Perspectives Are Shifting, But in What Direction?
All of this has started to open the window to different conversations surrounding effective addiction treatment. Programs relying solely on 12-step and abstinence-based models are regularly being called into question.
However, I am not yet seeing an attendant shift in the disease model of addiction. Conferences premised on non-disease models are still small, and advocates of this approach are still few and far between.
 I am on the board of Above and Beyond Family Recovery Center in Chicago, one of the most innovative treatment programs in the country. We focus on providing free, high-level outpatient treatment to Chicago’s homeless and disadvantaged, but we have had a hard time gaining the support of other treatment programs in the city because we do not focus solely on 12-step programming or disease models of treatment (although these are offered alongside our other programs).
I am on the board of Above and Beyond Family Recovery Center in Chicago, one of the most innovative treatment programs in the country. We focus on providing free, high-level outpatient treatment to Chicago’s homeless and disadvantaged, but we have had a hard time gaining the support of other treatment programs in the city because we do not focus solely on 12-step programming or disease models of treatment (although these are offered alongside our other programs).
 Americans have a long history of deterministic thinking when it comes to human behavior. Starting with Calvinistic predeterminism in colonial America and then evolving into Eugenics, the American view of genetic influences rarely goes beyond a limited and simplistic notion of Mendel’s pea experiments (perhaps a topic for a future blog post).
Americans have a long history of deterministic thinking when it comes to human behavior. Starting with Calvinistic predeterminism in colonial America and then evolving into Eugenics, the American view of genetic influences rarely goes beyond a limited and simplistic notion of Mendel’s pea experiments (perhaps a topic for a future blog post).
With this misconception, most Americans still view addiction as some kind of genetically predetermined disease, one that is chronic, progressive and incurable.
In the context of our conversation here, MAT is seen as some kind of fix for an ingrained defect, one that perhaps rebalances out-of-whack or deficient  neurochemicals in the brain. What most Americans have not yet grasped is that MAT, or any other substance that alters the brain’s neurochemicals, simply combats symptoms, which is not so different from how cold medicines alleviate symptoms rather than cure the actual cold. The key difference here is that OUD symptoms induce so much suffering that users are often driven to continue using. Opioids are of course the best (if not only) way to control opioid withdrawal symptoms. In this respect, relieving symptoms, though not a cure, can change behavior patterns that exacerbate the underlying problem.
neurochemicals in the brain. What most Americans have not yet grasped is that MAT, or any other substance that alters the brain’s neurochemicals, simply combats symptoms, which is not so different from how cold medicines alleviate symptoms rather than cure the actual cold. The key difference here is that OUD symptoms induce so much suffering that users are often driven to continue using. Opioids are of course the best (if not only) way to control opioid withdrawal symptoms. In this respect, relieving symptoms, though not a cure, can change behavior patterns that exacerbate the underlying problem.
In order to truly find recovery, you must rewire the neurological pathways in the brain, which will, in turn, drive changes in neurochemical balances. Just as one cannot lose weight or get fit by taking a diet pill, individuals cannot overcome addiction by taking a prescription. The pill can help, but lasting behavioral change requires focused effort over extended periods of time, as Dr. Lewis has often pointed out.
It is only through an accurate understanding of the interplay between genes, environment, and human experience that we can create effective solutions which help individuals and communities. It’s a goal I strive towards every day and I hope others reading this will do the same. For a much more in-depth discussion on how unconscious processes involved in learning and development (rather than genes or choice) drive addictive behaviors, see my article You’re Thinking about Addiction and Choice All Wrong.
………………………………
Nick Jaworski is an internationally recognized executive in the field of behavioral health marketing and operational consulting, with experience building organizations world-wide. As the owner of Circle Social Inc., he has helped healthcare organizations perform turnarounds and accelerate growth. He and his team spend most of their days in and out of treatment programs across the country. They do extensive analysis of trends, observe programs, interview patients and families, and analyze data from marketing campaigns. Nick is an advisor to the board for The Behavioral Health Association of Providers, and is also on the board for one of the most innovative treatment programs in the country – Above and Beyond Recovery.


 In the beginning, I thrived through the social connections I developed. I felt understood, and supported for the first time in years. Following this initial connection to its members, I slowly began to accept other elements of the 12-step philosophy, allowing them to influence and shape my views on the nature of addiction and, in some ways, on my approach to life.
In the beginning, I thrived through the social connections I developed. I felt understood, and supported for the first time in years. Following this initial connection to its members, I slowly began to accept other elements of the 12-step philosophy, allowing them to influence and shape my views on the nature of addiction and, in some ways, on my approach to life.



 able to access these medications on demand—in hospitals, doctor’s offices, emergency rooms and syringe exchange programs…. No urines or counseling or abstinence from opioids or other substances should be required to get these drugs, just as those barriers are not imposed on people with other disorders who need medication.
able to access these medications on demand—in hospitals, doctor’s offices, emergency rooms and syringe exchange programs…. No urines or counseling or abstinence from opioids or other substances should be required to get these drugs, just as those barriers are not imposed on people with other disorders who need medication. Simultaneously…many doctors have
Simultaneously…many doctors have  The result is tens of thousands of patients—many of whom were formerly medically stable—being left in pain, increased disability and withdrawal.
The result is tens of thousands of patients—many of whom were formerly medically stable—being left in pain, increased disability and withdrawal.  into care for those who decide they do want additional help…If you are successfully managing any ongoing mental health issues, you don’t need to keep showing up at a clinic.
into care for those who decide they do want additional help…If you are successfully managing any ongoing mental health issues, you don’t need to keep showing up at a clinic. In order to save lives, we need safer consumption spaces (or better yet, call them “overdose prevention sites”) in areas where drug use and sales are concentrated…
In order to save lives, we need safer consumption spaces (or better yet, call them “overdose prevention sites”) in areas where drug use and sales are concentrated… We also need shelters and housing, separate from those aimed at stabilization and abstinence, for people who are actively addicted, many of whom are also mentally ill and have symptoms related to severe trauma. When people have safe places to live and to use drugs, they are both much more likely to survive and much more likely to find ways to sustained recovery.
We also need shelters and housing, separate from those aimed at stabilization and abstinence, for people who are actively addicted, many of whom are also mentally ill and have symptoms related to severe trauma. When people have safe places to live and to use drugs, they are both much more likely to survive and much more likely to find ways to sustained recovery. also tend to be based on a 12-step ideology, which is fine for those who find that pathway amenable, but not for those who don’t—and not when that ideology is interpreted to stigmatize and discourage medication use.
also tend to be based on a 12-step ideology, which is fine for those who find that pathway amenable, but not for those who don’t—and not when that ideology is interpreted to stigmatize and discourage medication use. current administration—it may soon be possible.
current administration—it may soon be possible.
 I was astonished by the luxury when I arrived, but still nervous about this life change. I was approached by a client who befriended me, giving me an education on the “how to screw the system” plan that most of the clients followed. I learned about abusing detox meds, how to act like the perfect client, and who to get real (illegal) drugs from, all within the first week.
I was astonished by the luxury when I arrived, but still nervous about this life change. I was approached by a client who befriended me, giving me an education on the “how to screw the system” plan that most of the clients followed. I learned about abusing detox meds, how to act like the perfect client, and who to get real (illegal) drugs from, all within the first week. like many others, placed me in a low-income area surrounded by drug activity. Imagine 50 people from all over the country who just want to get high in a house where drugs are right over the fence. Most clients hopped the fence every day, got high, and hooked up with girls (it was a coed rehab). It was chaos. Being insecure, I fell right in. We’d get caught, sent back to detox, loaded up on suboxone and benzos (detox meds we’d get high on) and start treatment all over. The insurance billing cycle restarts and we would too. These types of centers benefit if you relapse because they can bill your insurance at a higher level of care.
like many others, placed me in a low-income area surrounded by drug activity. Imagine 50 people from all over the country who just want to get high in a house where drugs are right over the fence. Most clients hopped the fence every day, got high, and hooked up with girls (it was a coed rehab). It was chaos. Being insecure, I fell right in. We’d get caught, sent back to detox, loaded up on suboxone and benzos (detox meds we’d get high on) and start treatment all over. The insurance billing cycle restarts and we would too. These types of centers benefit if you relapse because they can bill your insurance at a higher level of care. sober living house, attempted AA, but continued to relapse. I still needed some real therapy. As time continued, I met more experienced users, got into new drugs, and learned more about how to use rehabs and detoxes to support my addiction.
sober living house, attempted AA, but continued to relapse. I still needed some real therapy. As time continued, I met more experienced users, got into new drugs, and learned more about how to use rehabs and detoxes to support my addiction. covered) high on opioid-benzo detox cocktails. When I really needed a reset, I would check into luxury treatment centers to get food, sleep and “work the system.” My insurance was great, and I found sober living homes that welcomed me to live there for free and get high, as long as I attended their outpatient rehab program. Treatment centers got paid for every relapse, and my addiction got worse. I knew I needed something more. I had to get away from this lifestyle of rehab hopping. There had to be something different.
covered) high on opioid-benzo detox cocktails. When I really needed a reset, I would check into luxury treatment centers to get food, sleep and “work the system.” My insurance was great, and I found sober living homes that welcomed me to live there for free and get high, as long as I attended their outpatient rehab program. Treatment centers got paid for every relapse, and my addiction got worse. I knew I needed something more. I had to get away from this lifestyle of rehab hopping. There had to be something different. negative thinking patterns. Places that used alternative approaches to therapy, such as SMART recovery, Rational Emotive Behavior Therapy, fitness therapy, and other critical thinking techniques to heal an addicted brain. For an analytical, physically broken person like me, this sounded like what I needed. I was guided to a place called Tree House Recovery in California, which offered this alternative approach.
negative thinking patterns. Places that used alternative approaches to therapy, such as SMART recovery, Rational Emotive Behavior Therapy, fitness therapy, and other critical thinking techniques to heal an addicted brain. For an analytical, physically broken person like me, this sounded like what I needed. I was guided to a place called Tree House Recovery in California, which offered this alternative approach. began to love life sober. I would highly recommend exploring
began to love life sober. I would highly recommend exploring 
 While grief or money woes can cause depression at any stage of life, there are specific factors that make older people who experience depression more vulnerable to addiction, which in turn may be harder to treat.
While grief or money woes can cause depression at any stage of life, there are specific factors that make older people who experience depression more vulnerable to addiction, which in turn may be harder to treat. Doctors are often willing to prescribe these potentially addictive drugs for sleep problems or for vague aches and pains. They also may not spot a developing addiction because it’s too easy to misdiagnose declining mental ability or a dishevelled appearance as being due to depression or dementia rather than substance use.
Doctors are often willing to prescribe these potentially addictive drugs for sleep problems or for vague aches and pains. They also may not spot a developing addiction because it’s too easy to misdiagnose declining mental ability or a dishevelled appearance as being due to depression or dementia rather than substance use. Drug addiction is especially dangerous because our metabolism slows as we age. Substances take longer to filter through the liver and may build up in the body. This puts older adults at greater risk of dangerous side effects or accidental overdoses.
Drug addiction is especially dangerous because our metabolism slows as we age. Substances take longer to filter through the liver and may build up in the body. This puts older adults at greater risk of dangerous side effects or accidental overdoses. Yet older adults deserve the option to seek treatment if they want help with a substance use disorder. Just like younger people, they can and do overcome addictions with proper counselling and support.
Yet older adults deserve the option to seek treatment if they want help with a substance use disorder. Just like younger people, they can and do overcome addictions with proper counselling and support.