Since retiring from the university about a month ago, my “career” seems to be better defined than ever. I’m a science writer and a speaker. And because I get invited to write articles and give talks, I’m obliged to continue to update my understanding of my field, which happens to be addiction.
And things keep changing. In the realm of neuroscience, there is more attention to neuroplasticity, more attention to cellular changes and the molecules involved, new findings in genetics, epigenetics, the biological sequels of early trauma, and so much more. In the treatment realm, harm reduction and decriminalization have become centre stage,  there is increasing opposition to court-ordered attendance at 12-step groups, and the glaring discrepancy between the brain disease model and 12-step methods continues to…well, glare. At the interface between science and treatment, there’s new thinking about the benefits of psychedelics, new research on how meditation changes the brain, investigation of smartphone apps that might help control urges, and increasing precision in the debate between the disease model and the learning model — as both sides advance their weaponry.
there is increasing opposition to court-ordered attendance at 12-step groups, and the glaring discrepancy between the brain disease model and 12-step methods continues to…well, glare. At the interface between science and treatment, there’s new thinking about the benefits of psychedelics, new research on how meditation changes the brain, investigation of smartphone apps that might help control urges, and increasing precision in the debate between the disease model and the learning model — as both sides advance their weaponry.
I want to do a few posts that identify and explore these new directions.
To start, let’s go back to the fundamental question of definition. If addiction isn’t a disease, then what is it? As you can imagine, I get asked this a lot.
My first reaction is to call addiction a habit of mind. But what on earth does that mean? Calling it a habit of mind at least avoids having to choose to focus on cognition, emotion, or behaviour: rather, all three are on the table. Which respects the  finding that cognition, emotion, and behaviour can’t be clearly differentiated in brain structure or function. They overlap entirely.
finding that cognition, emotion, and behaviour can’t be clearly differentiated in brain structure or function. They overlap entirely.
But what do I mean by habit? It’s an old word, a colloquial word…how much traction can we get from such an everyday term?
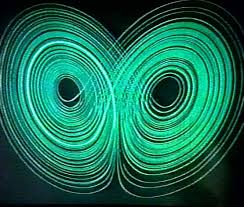
 To explore that question, let me tell you how scientists define a habit. And for that, we need to take a brief tour of complexity theory. According to complexity theory, a habit is a stable state in a complex system — a system composed of many interacting parts. Complex systems — such as ecosystems, societies, cultures, family dynamics, flocks of birds, herds of cattle, individual minds, individual bodies, and certainly individual brains — are made up of components (birds in a flock, family members at the
To explore that question, let me tell you how scientists define a habit. And for that, we need to take a brief tour of complexity theory. According to complexity theory, a habit is a stable state in a complex system — a system composed of many interacting parts. Complex systems — such as ecosystems, societies, cultures, family dynamics, flocks of birds, herds of cattle, individual minds, individual bodies, and certainly individual brains — are made up of components (birds in a flock, family members at the  dinner table, plants and animals in an ecosystem) that continue to influence each other. As a result, the relations between them continue to change, which means that the whole system (e.g., the family, the flock, the body, the mind) can continue to alter its form. Change is intrinsic; it doesn’t come from outside the system. Change means change in the interaction patterns, the relationship of the components, not the components themselves.
dinner table, plants and animals in an ecosystem) that continue to influence each other. As a result, the relations between them continue to change, which means that the whole system (e.g., the family, the flock, the body, the mind) can continue to alter its form. Change is intrinsic; it doesn’t come from outside the system. Change means change in the interaction patterns, the relationship of the components, not the components themselves.
 Your sister makes a caustic remark at the dinner table, then your mother puts down her fork, and then your father gets silent and distant, and then Aunt Jenny starts to criticize your sister. So the shape or form of the family dynamic changes, all by itself, with no particular push from the outside world.
Your sister makes a caustic remark at the dinner table, then your mother puts down her fork, and then your father gets silent and distant, and then Aunt Jenny starts to criticize your sister. So the shape or form of the family dynamic changes, all by itself, with no particular push from the outside world.
But if complex systems can change so easily, why do they tend to fall into the same familiar patterns time after time? In fact, stable, recurrent patterns — or “habits” — are fundamental to all complex systems. They are called attractors, because they literally “attract” the system. The flock of birds continues to fall into its characteristic V shape, family arguments always devolve into a familiar but infuriating script, and individual minds fall into familiar concerns or interpretations (e.g., “nobody really understands me!” or “I’m just so cool”) every hour of every day. Attractors aren’t necessarily attractive!
When we talk about people’s minds, what do we generally call these attractors — these habits of mind? Well, if they last only a few hours, we can call them moods. But if they recur week after week, month after month, year after year, we can call  them personality patterns. Personality patterns (or traits) emerge more and more predictably during childhood and adolescence. (Of course, most people have several and can even be seen switching from one to another — e.g., grumpiness to guilt — as circumstances shift.) These patterns recur, they get reinforced, they set synaptic connections into particular configurations (or recurring synaptic configurations set them, depending on how you look at it), and
them personality patterns. Personality patterns (or traits) emerge more and more predictably during childhood and adolescence. (Of course, most people have several and can even be seen switching from one to another — e.g., grumpiness to guilt — as circumstances shift.) These patterns recur, they get reinforced, they set synaptic connections into particular configurations (or recurring synaptic configurations set them, depending on how you look at it), and  they stabilize. In fact they become incredibly stable. Traits consolidate with development and they perpetuate themselves, becoming “stuck” over the lifespan.
they stabilize. In fact they become incredibly stable. Traits consolidate with development and they perpetuate themselves, becoming “stuck” over the lifespan.
Complex systems naturally fall into habits. Otherwise, they would waste a lot of energy trying and discarding different patterns, different forms. That’s called chaos, and nature doesn’t like chaos. Complex systems fall apart if they can’t cohere into patterns. In fact, a large-scale pattern actually maintains the interaction of its parts in a very particular (and energy-efficient) configuration, which recreates the large-scale pattern again and again. So the (global) pattern and the (local) interactions literally cause each other (called circular causality). That’s what makes habits so resilient.  That’s why it’s so hard to achieve deep, lasting change through psychotherapy. Hard, but not impossible.
That’s why it’s so hard to achieve deep, lasting change through psychotherapy. Hard, but not impossible.
What does this have to do with addiction? As I see it, personality traits or habits include what we might consider mental health problems. Such as: depression, anxiety disorder, overdependency,  paranoia, obsessive-compulsive disorder, aggressive or antisocial personality style, etc, etc. All those patterns emerge and stabilize over development (even if they get a boost from genetics). They usually become stuck by early adulthood, they cause a lot of misery, and they are hard (but not impossible) to change. Addiction is just another such pattern.
paranoia, obsessive-compulsive disorder, aggressive or antisocial personality style, etc, etc. All those patterns emerge and stabilize over development (even if they get a boost from genetics). They usually become stuck by early adulthood, they cause a lot of misery, and they are hard (but not impossible) to change. Addiction is just another such pattern.
So addiction isn’t really different from other mental health issues: it’s a sticky, long-lasting habit in the development of the self. And when you look at how complex systems work, how they get stuck, you see that addiction is actually natural. It’s not some kind of aberration. (Of course that doesn’t mean it’s good!)
Addiction is a habit in a very real sense. It’s a self-perpetuating way of thinking, a self-cohering set of beliefs, a self-reinforcing progression of emotions (desire-excitement-disappointment), and a limited (stuck) behavioural repertoire. Addiction is a habit of mind.

 Currently, only medical marijuana is legal in Canada under its
Currently, only medical marijuana is legal in Canada under its  to medical marijuana only through licensed producers with a medical document signed by an authorized healthcare practitioner.
to medical marijuana only through licensed producers with a medical document signed by an authorized healthcare practitioner. Yet it is interesting to note that some smokers may experience withdrawal
Yet it is interesting to note that some smokers may experience withdrawal  symptoms that can cause a
symptoms that can cause a  imprisonment. Possession of marijuana penalties range from a 6 month and $1000 fine (for up to 30 g) to 5 years less a day in prison.
imprisonment. Possession of marijuana penalties range from a 6 month and $1000 fine (for up to 30 g) to 5 years less a day in prison. author’s law firm) has put together
author’s law firm) has put together  From the Netherlands, which allows users to smoke in openly accepted, though illegal, marijuana cafes, to Portugal, where all drugs were decriminalized and addiction treatment programs aggressively implemented, the infographic explores the nuances in soft drug policies. In the USA, though five states have legalized marijuana medically and recreationally, it still has yet to be fully legalized across the country.
From the Netherlands, which allows users to smoke in openly accepted, though illegal, marijuana cafes, to Portugal, where all drugs were decriminalized and addiction treatment programs aggressively implemented, the infographic explores the nuances in soft drug policies. In the USA, though five states have legalized marijuana medically and recreationally, it still has yet to be fully legalized across the country.

 to have a NTX implant, to increase the chances that they would get through the crucial and often difficult first couple of months, when relapse rates are highest. We did around 2000 home detoxes before one family fatally misunderstood the instructions. Naturally, I feel bad about that but I don’t feel bad about trying to devise affordable treatment. I think that case made the difference between a reprimand and being removed from the register, but many addiction clinicians and academics in Britain (and several abroad who gave evidence for me) will tell you that the establishment were out to get me and were looking for excuses.
to have a NTX implant, to increase the chances that they would get through the crucial and often difficult first couple of months, when relapse rates are highest. We did around 2000 home detoxes before one family fatally misunderstood the instructions. Naturally, I feel bad about that but I don’t feel bad about trying to devise affordable treatment. I think that case made the difference between a reprimand and being removed from the register, but many addiction clinicians and academics in Britain (and several abroad who gave evidence for me) will tell you that the establishment were out to get me and were looking for excuses. If Marc thinks I look a bit weird in some of the online images, that’s probably because they were taken when I was trying to force my way through a rat-pack of paparazzi after the final hearing. Fortunately, the clinic I set up continues and is still doing most of the things that we had been doing up to the hearings. Some of those — e.g. using slow-release morphine for people who don’t get on well with methadone or buprenorphine — are now pretty normal, at least outside the USA. The clinic is also expanding its patient groups to include the growing problem — though it’s still small by US standards — of prescription opiate abuse and the management of ‘therapeutic addiction’ to opiates in pain problems. I only have an advisory role these days but we hope to extend what Emmanuel and I suggested should be called ‘Antagonist-Assisted Abstinence’ (AAA – geddit?) to benzodiazepines. Using s/c or slow i/v flumazenil infusions, it’s quite easy to take people off fistfuls of diazepam and other benzodiazepines in five days with very little discomfort, and a flumazenil implant is being developed in Australia.
If Marc thinks I look a bit weird in some of the online images, that’s probably because they were taken when I was trying to force my way through a rat-pack of paparazzi after the final hearing. Fortunately, the clinic I set up continues and is still doing most of the things that we had been doing up to the hearings. Some of those — e.g. using slow-release morphine for people who don’t get on well with methadone or buprenorphine — are now pretty normal, at least outside the USA. The clinic is also expanding its patient groups to include the growing problem — though it’s still small by US standards — of prescription opiate abuse and the management of ‘therapeutic addiction’ to opiates in pain problems. I only have an advisory role these days but we hope to extend what Emmanuel and I suggested should be called ‘Antagonist-Assisted Abstinence’ (AAA – geddit?) to benzodiazepines. Using s/c or slow i/v flumazenil infusions, it’s quite easy to take people off fistfuls of diazepam and other benzodiazepines in five days with very little discomfort, and a flumazenil implant is being developed in Australia. months off for withdrawal — are being put on forced reductions. I never claimed to be perfect (as we say in the trade, ‘if you haven’t made any mistakes. you’re not seeing enough patients’) but I don’t think that anything I did caused remotely as much misery and disaster to opiate addicts as the policies encouraged by the addiction establishment in the face of mounting evidence for the value of methadone-maintenance treatment.
months off for withdrawal — are being put on forced reductions. I never claimed to be perfect (as we say in the trade, ‘if you haven’t made any mistakes. you’re not seeing enough patients’) but I don’t think that anything I did caused remotely as much misery and disaster to opiate addicts as the policies encouraged by the addiction establishment in the face of mounting evidence for the value of methadone-maintenance treatment.
 But the most interesting event of my trip was meeting a man named Colin Brewer. If you google him you’ll see that he’s a wild child in British psychiatry circles. Most recently he was villainized by the media for providing
But the most interesting event of my trip was meeting a man named Colin Brewer. If you google him you’ll see that he’s a wild child in British psychiatry circles. Most recently he was villainized by the media for providing  supportive assessments
supportive assessments  We wasted no time discussing whether addiction was a disease or not. We both saw the classic disease model as a dead-end. Rather, we talked about the power of placebos, the extent to which addiction includes placebo-like effects — namely the belief that taking something has particular benefits, when the belief creates the benefits. Colin introduced me to a study showing that even physical withdrawal symptoms can follow sudden termination of a placebo believed to be an addictive drug. Fascinating!
We wasted no time discussing whether addiction was a disease or not. We both saw the classic disease model as a dead-end. Rather, we talked about the power of placebos, the extent to which addiction includes placebo-like effects — namely the belief that taking something has particular benefits, when the belief creates the benefits. Colin introduced me to a study showing that even physical withdrawal symptoms can follow sudden termination of a placebo believed to be an addictive drug. Fascinating!

 or to our community. We want the resulting ambivalence and cognitive dissonance to go away. So we put the addiction in a compartment, over to the side in our psyche. A little box of respite and relief when we need it, and no one else needs to know about it or disapprove.
or to our community. We want the resulting ambivalence and cognitive dissonance to go away. So we put the addiction in a compartment, over to the side in our psyche. A little box of respite and relief when we need it, and no one else needs to know about it or disapprove. Our recovery is under control: it’s in a box. But unlike addiction, our recovery compartment doesn’t usually leak. It just sits there. It doesn’t become the central part of our daily life that the addiction was. In fact, with recovery, compartmentalization poses the opposite threat: the danger that it may dry up and disappear if left in its box.
Our recovery is under control: it’s in a box. But unlike addiction, our recovery compartment doesn’t usually leak. It just sits there. It doesn’t become the central part of our daily life that the addiction was. In fact, with recovery, compartmentalization poses the opposite threat: the danger that it may dry up and disappear if left in its box. leaves a very big hole that something else needs to fill. If nothing fills that hole, whatever it is we quit is going to come back. A compartmentalized approach to recovery is not enough to allow the strands of workable change, the tendrils of real transformation, to be established and maintained.
leaves a very big hole that something else needs to fill. If nothing fills that hole, whatever it is we quit is going to come back. A compartmentalized approach to recovery is not enough to allow the strands of workable change, the tendrils of real transformation, to be established and maintained. can troubleshoot and collaborate to solve problems as they arise. There is the feeling that we are all in this together, all on the same team. When we feel this way, alienation tends to dissolve, and the need to compartmentalize, to control, lightens up. It’s safe for our recovery to emerge from its box, like a butterfly from its cocoon.
can troubleshoot and collaborate to solve problems as they arise. There is the feeling that we are all in this together, all on the same team. When we feel this way, alienation tends to dissolve, and the need to compartmentalize, to control, lightens up. It’s safe for our recovery to emerge from its box, like a butterfly from its cocoon.