…and how modern society fails to meet them.
Hi everyone. I hope your summer is going smoothly, safe from insects, droughts, forest fires, and other human-assisted calamities. I’m on vacation in France now, after a harrowing trip giving talks, first in Victoria, Canada, and then in Melbourne and Brisbane. Harrowing because I flew across 16 time zones, then back, in just a week. But it was a great trip, the highlight of which was hanging out with inmates, then giving a talk, at a beautiful prison on Vancouver Island. I know the phrase “beautiful prison” is rare, but this was a rare place. It included an area for First  Nations rituals (complete with sweat lodge!), a Buddhist meditation parkette, and wild deer running everywhere. The only problem for the prisoners was that they couldn’t leave. The place was a living contradiction, and of course most inmates had been through addiction. A few of them gave me lovely gifts when I left. They spent their time developing craftsmanship in wood and metal. (And yes, I was allowed to leave — but I felt a familiar anxiety at the exit post, left over from years ago.)
Nations rituals (complete with sweat lodge!), a Buddhist meditation parkette, and wild deer running everywhere. The only problem for the prisoners was that they couldn’t leave. The place was a living contradiction, and of course most inmates had been through addiction. A few of them gave me lovely gifts when I left. They spent their time developing craftsmanship in wood and metal. (And yes, I was allowed to leave — but I felt a familiar anxiety at the exit post, left over from years ago.)
Now that the zillions of comments on April’s moving post have finally died down, here’s a “vacation post” — a shortened and revised version of an article I published in The Guardian about a month ago. I’ve been asked many times what I think about the opioid/overdose epidemic hitting the US and Canada in particular but also the UK and other regions. Here are my thoughts.
……….
Most drug-related deaths result from the use of opioids, the molecules that are marketed as painkillers by pharmaceutical companies and heroin by drug lords. Opioids comprise a large family of molecular cousins, some weak, some powerful, all united by their capacity to bond with the opioid receptors all over our bodies, particularly our brains. Those receptors evolved to protect us from panic, anxiety, and pain. But the gentle impact of natural opioids, produced by our own bodies, resembles a summer breeze compared to the hurricane of physiological disruption caused by drugs — opiates — designed to mimic their function. And as if heroin wasn’t enough of a bull in the China shop, most street opiates (including heroin) are now laced or replaced with  fentanyl and its analogues, far more powerful than heroin and so cheap that drug-dealing profits are skyrocketing at about the same rate as overdose deaths. People don’t know what they’re getting and they take too much. Fentanyl is recognized as a primary driver of the overdose epidemic.
fentanyl and its analogues, far more powerful than heroin and so cheap that drug-dealing profits are skyrocketing at about the same rate as overdose deaths. People don’t know what they’re getting and they take too much. Fentanyl is recognized as a primary driver of the overdose epidemic.
Society’s response has been understandably desperate but generally wrong-headed. We start by blaming addicts for their self-indulgence or weakness of will. We blame the pharmaceutical companies for  developing and marketing painkillers. We blame doctors, for overprescribing opiates, which pressures them to underprescribe them, which drives patients to street drugs — cheaper, home-delivery via the
developing and marketing painkillers. We blame doctors, for overprescribing opiates, which pressures them to underprescribe them, which drives patients to street drugs — cheaper, home-delivery via the  internet, and zero quality control. We say we’re going to rekindle the war on drugs, recognized by experts as a colossal failure from the thirties onward. Dealers will always find their way to consumers if the price is right. We also continue to view addiction as a chronic brain disease, so the benefits of education, social support, and psychological intervention receive far too little attention. Black-and-white solutions are simply inadequate for a problem of such complexity.
internet, and zero quality control. We say we’re going to rekindle the war on drugs, recognized by experts as a colossal failure from the thirties onward. Dealers will always find their way to consumers if the price is right. We also continue to view addiction as a chronic brain disease, so the benefits of education, social support, and psychological intervention receive far too little attention. Black-and-white solutions are simply inadequate for a problem of such complexity.
There has been some progress: There are pockets of activity here and there where prescribed opiates — like methadone and buprenorphine (Suboxone) — are made more easily available to addicts. That’s a good thing, because increasing addicts’ desperation (e.g., methadone clinic line-ups on the far side of town) often drives  them to the street, where they’re most likely to die. The availability of naloxone, an opiate neutralizer, is slowly wending its way through the drug policy jungle, providing a simple resource to combat overdose on the spot. But in most segments of most communities in the US and elsewhere, naloxone is still too difficult to obtain.
them to the street, where they’re most likely to die. The availability of naloxone, an opiate neutralizer, is slowly wending its way through the drug policy jungle, providing a simple resource to combat overdose on the spot. But in most segments of most communities in the US and elsewhere, naloxone is still too difficult to obtain.
I think there are smarter answers at hand — but also smarter questions to be asked. The opioid overdose epidemic compels us to face one of the darkest corners of modern human experience head on, to stop wasting time blaming the players and start looking directly at the source of the problem. What does it feel like to be a human trying to make it in the early 21st century? Why are we so stressed out that our own (internal) supply of opioids isn’t enough to feel okay?
The overdose crisis obviously builds on people’s desire for opioids. But what do opioids actually do? The opioid system was designed by evolution to allow us to function, not panic or shut down, when we are under threat or in pain. Critically, support from other humans also helps us cope with stress, and that support is underpinned by  opioids too. Our attachment to others, whether in friendship, family, or romance, requires opioid metabolism so that we can feel the love. Opioids grant us a sense of warmth and safety when we connect with each other. You get opioids (from your own brain stem) when you get a hug. Breast milk is rich with opioids. Rodents play more when given mild doses of opioids.
opioids too. Our attachment to others, whether in friendship, family, or romance, requires opioid metabolism so that we can feel the love. Opioids grant us a sense of warmth and safety when we connect with each other. You get opioids (from your own brain stem) when you get a hug. Breast milk is rich with opioids. Rodents play more when given mild doses of opioids.
 In short, we need opioids to feel safe and to connect with each other. Then what does it say about our life-style if our natural supply isn’t sufficient? It says we are stressed and isolated. That’s a problem we need to resolve.
In short, we need opioids to feel safe and to connect with each other. Then what does it say about our life-style if our natural supply isn’t sufficient? It says we are stressed and isolated. That’s a problem we need to resolve.
To confront the problem of addiction, many have proposed targeted education, community support, and interpersonal bonding through group activities. Johann Hari’s powerful book, Chasing the Scream, reviews how such initiatives have worked in diverse societies. An intriguing example is the compassionate, blame-free dialogue that has naturally evolved among high-school students in Portugal, highlighting the dangers of hard drugs and urging the most vulnerable to abstain — not because they’re going to get in trouble but because addiction is miserable and dangerous! The emergence of this dialogue has been particularly meaningful because it has paralleled the decriminalization of drug use. Portugal had an astoundingly high heroin addiction rate 17 years ago. It now boasts the second lowest overdose rate on the continent. Drug addiction has diminished significantly in Portugal because compassion and social inclusion actually work against addiction, while punishment only fuels it.
But let’s look beyond the challenge of addiction per se. The peculiar appeal of opioids tells us more about ourselves as a society, as a culture, than addiction statistics can reveal. Today’s young people come of age and carve out their adult lives in an environment of astronomical uncertainty. Corporations that used to pride themselves on fairness to their employees now strive only for profit. The echelons of management are as risk-infected as those of the lowest clerks. Massive layoffs rationalized by the eddies of globalization make long-term  contracts antique. I ask the guys who come to the house to deliver packages or upgrade our TV box how they like their jobs. They can’t say. They get up to three six-month contracts in a row and then they get laid off so the company won’t have to pay them benefits. People pour out of colleges and universities with all manner of degrees, yet with skills that are rapidly becoming irrelevant. But people without those degrees are
contracts antique. I ask the guys who come to the house to deliver packages or upgrade our TV box how they like their jobs. They can’t say. They get up to three six-month contracts in a row and then they get laid off so the company won’t have to pay them benefits. People pour out of colleges and universities with all manner of degrees, yet with skills that are rapidly becoming irrelevant. But people without those degrees are  even worse off. They find themselves virtually unemployable, because there are so many others in the same pool, and employers will hire whoever comes cheapest. (The absurdly low minimum wage figures in the US clearly exacerbate the situation.) As hope for steady employment fizzles, so does the opportunity to connect with family, friends, and society more broadly, and there is way too much time to kill. Opioids help reduce the despair.
even worse off. They find themselves virtually unemployable, because there are so many others in the same pool, and employers will hire whoever comes cheapest. (The absurdly low minimum wage figures in the US clearly exacerbate the situation.) As hope for steady employment fizzles, so does the opportunity to connect with family, friends, and society more broadly, and there is way too much time to kill. Opioids help reduce the despair.
The opportunity to settle into a viable niche in one’s family and one’s society, the bedrock of social and personal security, is being blown away by the winds of unregulated capitalism in a globalized world. As for the intimacy and trust we humans have always sought in each other, in friends, colleagues, and lovers, the bonds are shaky these days. Even if we have the opportunity to connect — if we are not resettling geographically to find employment or staying up late to retool through distance education or simply sitting on the sofa all day long collecting welfare — we’re still too stressed and depressed to get to know each other, to develop trust, to give and receive compassion.
(The links between under-employment, family dissolution, and addiction are beautifully reviewed by Sally Satel. And many of you may know of Bruce Alexander’s explanation of how globalization feeds addiction.)
The early 21st century offers less structure and stability through religion, and through extended family relationships, than we have experienced in thousands of years. And maybe that’s just the way it is. But we don’t have to throw away the basic currency of security and interconnectedness entirely. We can build social structures — governments, corporations, community organizations, and systems of education and care — that encourage stability, hope, and trust in our day-to-day lives. Like the high-school kids in Portugal, we can offer compassion and inclusion as an alternative to heroin. If we fail to do that, many of us will want to hook ourselves up to an opioid pump. Just to endure.
……..
I’m not entirely pessimistic, but that’s the way I see it. Regardless, let’s not give up hope, not even slightly. Let’s do a bit of meditation, enjoy the sunshine, and be good to each other. See you again in September.
 policies over the last many years: opposition to raising the minimum wage, opposition to universal health care, guns for all, reduced taxation on the wealthy, training people to blame others for their misfortunes rather than look at the elephant (pun intended) in the room.
policies over the last many years: opposition to raising the minimum wage, opposition to universal health care, guns for all, reduced taxation on the wealthy, training people to blame others for their misfortunes rather than look at the elephant (pun intended) in the room. something strong, powered by defiance. Consequences be damned. It’s sort of the ultimate “fuck you” directed at…well directed at the adults upstairs….Obama, Hillary….the adults who seem somehow to be responsible for whatever pain we’re feeling.
something strong, powered by defiance. Consequences be damned. It’s sort of the ultimate “fuck you” directed at…well directed at the adults upstairs….Obama, Hillary….the adults who seem somehow to be responsible for whatever pain we’re feeling.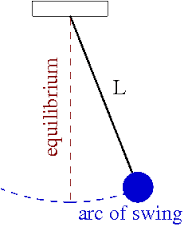 Sometimes a sick system needs a chance to swing all the way wrong before the pendulum reverses its direction. Maybe with a Republican president and Congress, legislation, policy, the courts will have had a full run, their unfettered chance to make things as wrong as possible — and then things will swing back leftward. Because there won’t be anyone to blame and because the politics of selfishness and fear are unstable — they can’t last indefinitely.
Sometimes a sick system needs a chance to swing all the way wrong before the pendulum reverses its direction. Maybe with a Republican president and Congress, legislation, policy, the courts will have had a full run, their unfettered chance to make things as wrong as possible — and then things will swing back leftward. Because there won’t be anyone to blame and because the politics of selfishness and fear are unstable — they can’t last indefinitely.

 Nations rituals (complete with sweat lodge!), a Buddhist meditation parkette, and wild deer running everywhere. The only problem for the prisoners was that they couldn’t leave. The place was a living contradiction, and of course most inmates had been through addiction. A few of them gave me lovely gifts when I left. They spent their time developing craftsmanship in wood and metal. (And yes, I was allowed to leave — but I felt a familiar anxiety at the exit post, left over from years ago.)
Nations rituals (complete with sweat lodge!), a Buddhist meditation parkette, and wild deer running everywhere. The only problem for the prisoners was that they couldn’t leave. The place was a living contradiction, and of course most inmates had been through addiction. A few of them gave me lovely gifts when I left. They spent their time developing craftsmanship in wood and metal. (And yes, I was allowed to leave — but I felt a familiar anxiety at the exit post, left over from years ago.)
 developing and marketing painkillers. We blame doctors, for overprescribing opiates, which pressures them to underprescribe them, which drives patients to street drugs — cheaper, home-delivery via the
developing and marketing painkillers. We blame doctors, for overprescribing opiates, which pressures them to underprescribe them, which drives patients to street drugs — cheaper, home-delivery via the  internet, and zero quality control. We say we’re going to
internet, and zero quality control. We say we’re going to  them to the street, where they’re most likely to die. The availability of naloxone, an opiate neutralizer, is slowly wending its way through the drug policy jungle, providing a simple resource
them to the street, where they’re most likely to die. The availability of naloxone, an opiate neutralizer, is slowly wending its way through the drug policy jungle, providing a simple resource  opioids too. Our attachment to others, whether in friendship, family, or romance, requires opioid metabolism so that we can feel the love. Opioids grant us a sense of warmth and safety when we connect with each other. You get opioids (from your own brain stem) when you get a hug. Breast milk is rich with opioids. Rodents play more when given mild doses of opioids.
opioids too. Our attachment to others, whether in friendship, family, or romance, requires opioid metabolism so that we can feel the love. Opioids grant us a sense of warmth and safety when we connect with each other. You get opioids (from your own brain stem) when you get a hug. Breast milk is rich with opioids. Rodents play more when given mild doses of opioids. In short, we need opioids to feel safe and to connect with each other. Then what does it say about our life-style if our natural supply isn’t sufficient? It says we are stressed and isolated. That’s a problem we need to resolve.
In short, we need opioids to feel safe and to connect with each other. Then what does it say about our life-style if our natural supply isn’t sufficient? It says we are stressed and isolated. That’s a problem we need to resolve. contracts antique. I ask the guys who come to the house to deliver packages or upgrade our TV box how they like their jobs. They can’t say. They get up to three six-month contracts in a row and then they get laid off so the company won’t have to pay them benefits. People pour out of colleges and universities with all manner of degrees, yet with skills that are rapidly becoming irrelevant. But people without those degrees are
contracts antique. I ask the guys who come to the house to deliver packages or upgrade our TV box how they like their jobs. They can’t say. They get up to three six-month contracts in a row and then they get laid off so the company won’t have to pay them benefits. People pour out of colleges and universities with all manner of degrees, yet with skills that are rapidly becoming irrelevant. But people without those degrees are  even worse off. They find themselves virtually unemployable, because there are so many others in the same pool, and employers will hire whoever comes cheapest. (The absurdly low minimum wage figures in the US clearly exacerbate the situation.) As hope for steady employment fizzles, so does the opportunity to connect with family, friends, and society more broadly, and there is way too much time to kill. Opioids help reduce the despair.
even worse off. They find themselves virtually unemployable, because there are so many others in the same pool, and employers will hire whoever comes cheapest. (The absurdly low minimum wage figures in the US clearly exacerbate the situation.) As hope for steady employment fizzles, so does the opportunity to connect with family, friends, and society more broadly, and there is way too much time to kill. Opioids help reduce the despair. When I was 24 years old I went to the last of over a dozen treatment and detoxification centers I have attended. I was, and had always been, resistant to the 12-step approach to recovery, and I did not resonate with many of its underlying principles regarding the causes and treatment of addiction. But I followed the lead of some open-minded people at my last treatment center and began attending 12-step meetings voluntarily. And I began to recover. There is much that I learned from my 12-step involvement, the most important being the utilization of
When I was 24 years old I went to the last of over a dozen treatment and detoxification centers I have attended. I was, and had always been, resistant to the 12-step approach to recovery, and I did not resonate with many of its underlying principles regarding the causes and treatment of addiction. But I followed the lead of some open-minded people at my last treatment center and began attending 12-step meetings voluntarily. And I began to recover. There is much that I learned from my 12-step involvement, the most important being the utilization of  some kind of growth modality instead of simply trying to stop using. I also began identifying with others who had attachment wounds like mine, even if these concepts were not discussed overtly. I created some deep and lifelong friendships and learned about the fulfillment that comes from service to others. The Twelve Steps taught me that deep emotional change must be incrementally worked toward with diligence and sustained focus, and gave me a prescribed external structure (meetings,
some kind of growth modality instead of simply trying to stop using. I also began identifying with others who had attachment wounds like mine, even if these concepts were not discussed overtly. I created some deep and lifelong friendships and learned about the fulfillment that comes from service to others. The Twelve Steps taught me that deep emotional change must be incrementally worked toward with diligence and sustained focus, and gave me a prescribed external structure (meetings,  commitments, and step-work) upon which to start building these changes. Finally, in the beginning, it gave me a large group of people with whom I could openly share my struggles and successes, finally building a sense of personal competence and esteem.
commitments, and step-work) upon which to start building these changes. Finally, in the beginning, it gave me a large group of people with whom I could openly share my struggles and successes, finally building a sense of personal competence and esteem. by most members. I am also not remotely religious, and never attributed my ability to abstain to a higher power. Finally, and this became more apparent after I left 12-step involvement—especially after I incorporated moderate alcohol use into my life a few months later—listening to similar messages
by most members. I am also not remotely religious, and never attributed my ability to abstain to a higher power. Finally, and this became more apparent after I left 12-step involvement—especially after I incorporated moderate alcohol use into my life a few months later—listening to similar messages  repeatedly for years created a type of programming that made the idea of leaving difficult. To do so, I had to contend with deep feelings of fear caused by overt messages that leaving would inevitably lead to relapse and the loss of everything that I had spent so many years creating. Leaving also elicited deep feelings of shame and guilt that lasted acutely for months, and their tendrils still infect me two years later.
repeatedly for years created a type of programming that made the idea of leaving difficult. To do so, I had to contend with deep feelings of fear caused by overt messages that leaving would inevitably lead to relapse and the loss of everything that I had spent so many years creating. Leaving also elicited deep feelings of shame and guilt that lasted acutely for months, and their tendrils still infect me two years later. My addiction story is ruled by two deep, seemingly contradictory, truths: first, that deciding to become a 12-step member was one of the best decisions I’ve ever made. And second, that deciding to leave 12-step membership was one of the best decisions I’ve ever made. I wish that it weren’t anathema within the 12-step paradigm to leave either for periods or forever, but I kind of get it. I benefited from the same rigidity within 12-step doctrine that eventually repelled me. I may have temporarily needed that rigidity to counteract the evermore rigid attachment I had to heroin. I needed the external structure offered by the 12-step program and traditional abstinence until I could incorporate my own version of structure, inwardly. I needed form until I could safely find formlessness.
My addiction story is ruled by two deep, seemingly contradictory, truths: first, that deciding to become a 12-step member was one of the best decisions I’ve ever made. And second, that deciding to leave 12-step membership was one of the best decisions I’ve ever made. I wish that it weren’t anathema within the 12-step paradigm to leave either for periods or forever, but I kind of get it. I benefited from the same rigidity within 12-step doctrine that eventually repelled me. I may have temporarily needed that rigidity to counteract the evermore rigid attachment I had to heroin. I needed the external structure offered by the 12-step program and traditional abstinence until I could incorporate my own version of structure, inwardly. I needed form until I could safely find formlessness. Informed by unparalleled neuroscientific insight and written with his usual flare, Marc Lewis’s The Biology of Desire effectively refutes the medical view of addiction as a brain disease. A bracing and informative corrective to the muddle that now characterizes public and professional discourse on this topic.” —Gabor Maté, M.D., author of In The Realm of Hungry Ghosts: Close Encounters With Addiction
Informed by unparalleled neuroscientific insight and written with his usual flare, Marc Lewis’s The Biology of Desire effectively refutes the medical view of addiction as a brain disease. A bracing and informative corrective to the muddle that now characterizes public and professional discourse on this topic.” —Gabor Maté, M.D., author of In The Realm of Hungry Ghosts: Close Encounters With Addiction
Recent Comments